Alopecia areata incognita is a rare and often misunderstood form of hair loss that causes sudden, diffuse shedding without the classic bald patches seen in other types of alopecia.
Because it mimics conditions such as telogen effluvium or androgenetic alopecia, it can be challenging to identify and treat.
This guide explores how to recognize its unique features, who is most affected, and what steps to take if you suspect you may have this condition. Early awareness is key to effective hair loss treatment and long-term hair recovery.
What Is Alopecia Areata Incognita?
Alopecia areata incognita (AAI) is a rare, diffuse variant of alopecia areata, a non-scarring autoimmune condition where the immune system mistakenly attacks hair follicles.
Unlike classic alopecia areata, which causes well-defined patches of hair loss, AAI presents as sudden, widespread shedding across the entire scalp without obvious bald spots.
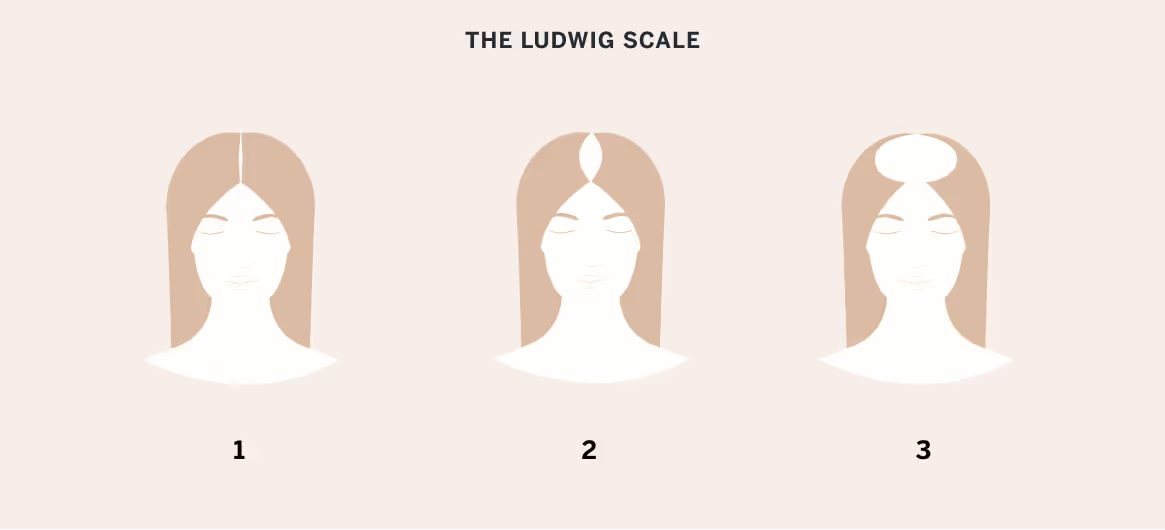
Because of its diffuse nature, AAI often mimics other types of hair loss, such as telogen effluvium or androgenetic alopecia, making diagnosis more complex. It tends to affect women more frequently, especially those between the ages of 20 and 40.
Despite the rapid shedding, hair follicles remain intact, meaning regrowth is often possible with appropriate treatment.
Trichoscopy and biopsy are usually required to confirm the diagnosis and rule out similar conditions.
How Alopecia Areata Incognita Differs From Other Types of Hair Loss
Alopecia areata incognita differs from typical alopecia areata in its presentation. Instead of patchy bald spots, patients experience rapid, diffuse thinning over the entire scalp.
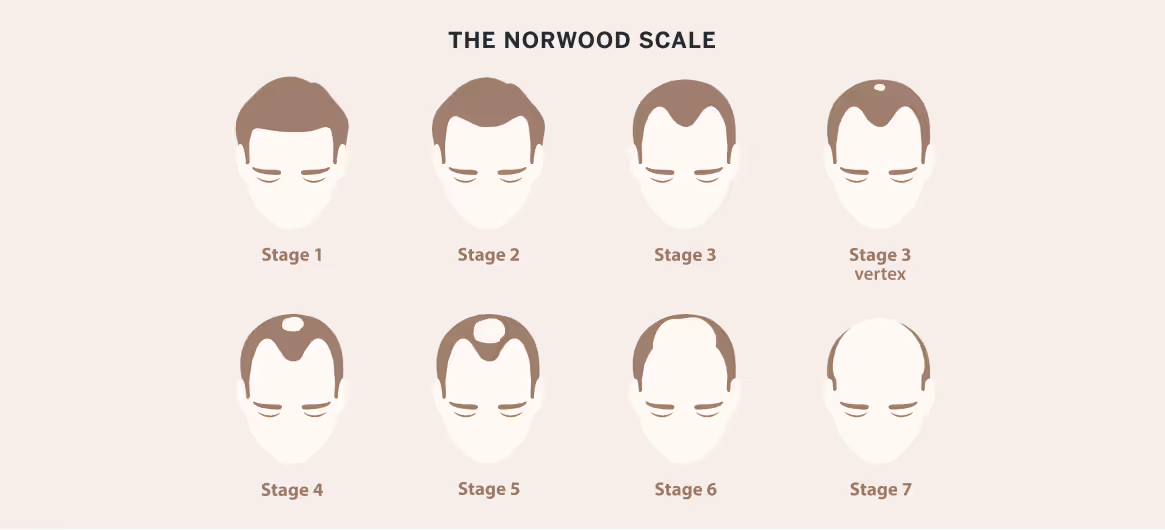
Unlike telogen effluvium, which is often self-limited and linked to a stressor, AAI is autoimmune and more persistent. It also lacks the patterned thinning seen in androgenetic alopecia.
Diagnosis relies on recognizing subtle signs, such as exclamation mark hairs or yellow dots, under trichoscopy that are not seen in other diffuse hair loss disorders.
Alopecia Areata Incognita vs. Diffuse Alopecia Areata
Alopecia areata incognita and diffuse alopecia areata both present with widespread hair thinning, but they differ in onset, duration, and clinical findings.
AAI typically causes abrupt, intense shedding with no visible patches, often resembling telogen effluvium. In contrast, diffuse alopecia areata may start more gradually, can appear over a prolonged period, and can progress to alopecia totalis (complete scalp hair loss) in some cases.
Trichoscopy in AAI reveals uniform findings such as yellow dots and miniaturized hairs, while diffuse alopecia areata may show more localized inflammation. Correctly distinguishing between them is essential for treatment planning and prognosis.
Who Is Most Likely To Get Alopecia Areata Incognita?
Alopecia areata incognita most commonly affects adult women, particularly those between the ages of 20 and 40. It is less frequently seen in men and rarely affects children.
Individuals with a personal or family history of autoimmune diseases, such as thyroid disorders or vitiligo, may be at increased risk.
AAI may also occur in those with a history of classical alopecia areata, though it can appear without any prior episodes. Stress and hormonal changes may be triggers.
Common Symptoms of Alopecia Areata Incognita
Alopecia areata incognita is characterized by sudden, diffuse hair thinning rather than distinct bald patches. Patients typically notice an alarming increase in daily hair shedding—often more than 100 hairs per day—especially while washing or brushing.
The scalp may appear less dense overall but without visible inflammation, scaling, or scarring. Unlike telogen effluvium, AAI may involve the loss of terminal (mature) hairs rather than mostly telogen hairs.
Trichoscopic findings such as yellow dots, exclamation mark hairs, and miniaturized hairs help distinguish it from other conditions.
Despite the rapid shedding, the scalp generally feels healthy without any tenderness. Eyebrow, eyelash, or body hair loss is rare in this form but may occur in more extensive cases.
Early Signs To Watch For
The earliest sign of alopecia areata incognita is sudden, excessive hair shedding that feels disproportionate to normal daily loss. Patients often report clumps of hair coming out during shampooing or noticeable hair left on pillows or clothing.
This increased shedding can occur without any clear trigger or recent illness. The hair density may look subtly reduced, especially on the crown or sides, but the scalp typically appears normal on visual inspection. Early recognition is critical for effective management.
How Symptoms Progress Over Time
If left untreated, AAI may progress from mild thinning to significant diffuse hair loss over weeks or months. The shedding can become chronic, leading to visibly reduced volume across the scalp.
Unlike other forms of alopecia, AAI rarely progresses to complete baldness, but the thinning can be distressing.
In some patients, hair regrowth begins spontaneously, though repeated cycles of shedding and regrowth are possible. Early intervention may shorten the course and improve long-term hair density.
When To See a Dermatologist
You should see a dermatologist if you experience sudden, unexplained hair shedding that lasts longer than a few weeks, especially if accompanied by reduced scalp density. Early evaluation is key to ruling out telogen effluvium, androgenetic alopecia, or other causes.
A dermatologist can perform a clinical exam, trichoscopy, and possibly a scalp biopsy to make an accurate diagnosis. Timely treatment can improve outcomes and may prevent further shedding or emotional distress associated with hair loss.
Diagnosing Alopecia Areata Incognita
Diagnosing alopecia areata incognita can be challenging due to its resemblance to other diffuse hair loss conditions.
Dermatologists typically begin with a thorough medical history, asking about recent stressors, illnesses, medications, family history of autoimmune disorders, and prior episodes of hair loss.
A physical exam of the scalp follows, often including a hair pull test. Diagnostic tools such as trichoscopy and, in some cases, scalp biopsy are used to confirm the diagnosis and differentiate AAI from telogen effluvium or androgenetic alopecia.
Clinical Examination and the Hair Pull Test
During the clinical exam, the dermatologist inspects the scalp for signs of inflammation, scarring, or miniaturization.
The hair pull test is a key step—several hairs are gently tugged to assess how many are easily released. In AAI, a positive pull test often reveals anagen or dystrophic hairs rather than telogen hairs.
Unlike scarring alopecias, the scalp appears healthy and intact. The presence of diffuse thinning without patchy bald spots often raises suspicion for AAI and guides further testing.

Trichoscopy and Scalp Biopsy
Trichoscopy—a noninvasive method using a dermatoscope—helps identify hallmark features of AAI.
Dermatologists may see yellow dots (indicating follicular keratin), exclamation mark hairs, short regrowing hairs, and tapered hairs. These findings are distinct from other diffuse alopecias.
If the diagnosis remains unclear, a scalp biopsy may be performed. Histopathology typically reveals peribulbar lymphocytic infiltration, or a “swarm of bees” appearance, confirming autoimmune activity.
Biopsies can also rule out scarring alopecia or telogen effluvium if clinical features are ambiguous.
Differentiating Telogen Effluvium and Androgenetic Alopecia
Alopecia areata incognita is frequently misdiagnosed as telogen effluvium or androgenetic alopecia due to its diffuse pattern. Telogen effluvium typically follows a stressor, affects telogen hairs, and resolves over months, while AAI often persists without a clear cause.
Androgenetic alopecia progresses slowly, often showing miniaturization and a patterned distribution. In contrast, AAI presents with abrupt shedding, exclamation mark hairs, and specific trichoscopic signs.
Careful examination and biopsy, when necessary, are essential for accurate differentiation and appropriate treatment.
Alopecia Areata Incognita in Men
While alopecia areata incognita (AAI) is more frequently diagnosed in women, it can and does affect men. However, its diffuse nature often makes it harder to identify in male patients, especially those who may already have early signs of androgenetic alopecia.
Because AAI does not follow a classic male-pattern baldness distribution, it may go unrecognized or be attributed to hereditary hair loss.
For men, the psychological impact can be profound, especially if hair loss occurs rapidly and without warning. Timely diagnosis is key to preventing unnecessary progression and helping preserve self-confidence.
Symptoms
In men, AAI typically presents as widespread, rapid thinning across the scalp rather than localized patches or a receding hairline. Unlike androgenetic alopecia, which begins with temples or crown thinning, AAI results in a uniform decrease in density.
Shedding is often abrupt and noticeable, with handfuls of hair lost during washing or grooming. The scalp usually appears normal, without inflammation or redness.
In some cases, thinning may be more prominent in the frontal region, but the absence of miniaturized hairs helps distinguish AAI from hereditary pattern baldness.
Unique Challenges for Male Patients
Men with AAI face unique challenges in both diagnosis and emotional impact. Because diffuse thinning may resemble early androgenetic alopecia, it’s often dismissed or misdiagnosed, which delays appropriate treatment.
Men may also feel societal pressure to minimize concern over hair loss, making them less likely to seek care early. Additionally, the rapid onset of thinning, especially when unexpected, can affect self-image, confidence, and mental well-being.
Addressing both the physical and psychological effects of AAI is essential to support male patients throughout diagnosis and treatment.
Causes and Risk Factors for Alopecia Areata Incognita
Alopecia areata incognita is considered a complex condition with multiple contributing factors.
While the exact cause is not always clear, it is generally understood to involve an inappropriate immune response targeting the hair follicles. However, the triggers that initiate this response can vary from person to person.
Understanding the underlying causes and risk factors is necessary not only for accurate diagnosis but also for developing a long-term management plan tailored to the individual's needs and health profile.
Genetics and Autoimmune Conditions
A family history of alopecia areata, autoimmune thyroid disease, vitiligo, or other autoimmune disorders increases the likelihood of developing the condition.
AAI itself is autoimmune in nature, meaning the body’s immune system mistakenly attacks its own hair follicles, disrupting normal hair growth.
This immune dysregulation can be influenced by inherited tendencies. Those with personal histories of autoimmune diseases, such as lupus, rheumatoid arthritis, or Hashimoto’s thyroiditis, are also more susceptible, making genetic and autoimmune links central to understanding AAI.
Triggers and Associated Health Conditions
Various internal and external triggers may precipitate the onset of alopecia areata incognita.
Common precipitating factors include viral infections (particularly upper respiratory infections), significant emotional stress, hormonal changes (such as those related to pregnancy or menopause), and certain medications.
Environmental exposures or immune-altering events may also act as catalysts. In some cases, the condition arises in conjunction with other health issues such as anemia, polycystic ovary syndrome (PCOS), or atopic dermatitis.
Some patients report flares following flu-like illnesses or during particularly stressful life periods. The timing typically shows a 2–3 month lag between trigger and hair loss onset.
Associated conditions extend beyond classic autoimmune diseases. Atopic conditions such as eczema, asthma, and allergic rhinitis occur more frequently in affected individuals.
Mental health correlations exist as well—anxiety and depression rates in those with alopecia areata incognita exceed general population levels, though whether these are causes or effects remains debated.
Nutritional deficiencies, particularly vitamin D, iron, and zinc, appear more common but might be consequences rather than causes.
Though a clear trigger is not always identifiable, understanding and managing potential contributing conditions can reduce recurrence and improve treatment outcomes.
Alopecia Areata Incognita Treatment Options
Because alopecia areata incognita is an autoimmune condition, treatment focuses on reducing inflammation, modulating immune response, and supporting hair regrowth. The approach varies depending on the severity and duration of hair loss.
While some cases resolve spontaneously, early intervention can shorten the shedding phase, improve regrowth, and reduce the risk of recurrence.
Topical and Intralesional Steroids
Topical corticosteroids are often the first line of treatment for AAI, particularly in cases with active shedding. High-potency steroids help suppress the immune attack on hair follicles and encourage regrowth. They are typically applied once or twice daily to the affected areas.
In more resistant or rapidly progressing cases, intralesional corticosteroid injections may be used. These are injected directly into the scalp in multiple small doses to target deeper inflammation.
Both methods can be effective, especially when initiated early, but require close monitoring to avoid side effects such as skin thinning or folliculitis.
Other Medical Therapies
When topical or intralesional steroids are insufficient, systemic therapies may be considered. Oral corticosteroids, such as prednisone, can provide more widespread immune suppression but are usually reserved for short-term use due to side effects.
In chronic or severe cases, immunomodulating agents such as methotrexate or cyclosporine may be prescribed. Newer treatments, including JAK inhibitors such as tofacitinib and baricitinib, have shown promising results in various forms of alopecia areata, including AAI.
These medications target immune signaling pathways involved in hair follicle attack. All systemic therapies require medical supervision and regular lab monitoring.
Supportive Care and Hair Regrowth Strategies

Supportive treatments are important for managing AAI and enhancing regrowth. Dermatologists may recommend minoxidil (available over the counter in topical form or by prescription for high-strength topical or oral forms) to stimulate hair follicles and promote faster recovery.
Nutritional support—including adequate levels of iron, vitamin D, and biotin—can also help optimize hair health, especially if underlying deficiencies exist.
Gentle hair care practices, avoiding excessive heat or chemical treatments, and stress-reduction techniques may support overall recovery.
While these approaches do not treat the autoimmune cause directly, they create a healthier environment for regrowth and minimize further hair damage.
Prognosis and Long-term Outlook
The prognosis for alopecia areata incognita is generally favorable, especially when diagnosed early and managed appropriately. Many patients experience full or substantial regrowth within several months, although the course can be unpredictable.
AAI is often a one-time event but may recur in some individuals, particularly those with autoimmune tendencies. The long-term outlook depends on how quickly treatment is initiated and whether underlying triggers can be identified and addressed.
Continued dermatologic follow-up is essential, as early detection of relapses improves the likelihood of rapid and complete recovery.
Living With Alopecia Areata Incognita
Living with alopecia areata incognita can feel overwhelming, especially when hair loss is sudden and unexplained, but it's important to remember that you're not alone and that help is available.
Many people with AAI go on to experience significant regrowth and emotional healing. With the right medical care, self-care strategies, and support systems, it's possible to manage the condition and maintain your confidence and well-being.
Coping With Emotional Impact and Hair Loss
The emotional toll of alopecia areata incognita can be as significant as the physical symptoms. Rapid hair loss often triggers anxiety, embarrassment, or feelings of lost identity. It’s important to acknowledge these emotions and seek support early.
Speaking with a mental health professional, practicing mindfulness, and engaging in activities that promote self-esteem can be beneficial. Some people find empowerment through hair styling choices, head coverings, or embracing their new appearance.
Open communication with loved ones and dermatologists can also reduce the sense of isolation.
Coping is a process, and compassionate self-care makes a meaningful difference.
Support Resources
A variety of resources are available. Support groups, both in-person and online, offer a space to share experiences, gain emotional validation, and learn from others facing similar challenges.
Organizations such as the National Alopecia Areata Foundation (NAAF) provide educational materials, advocacy opportunities, and community events. Dermatologists can also connect patients with counselors or trichologists who specialize in hair loss.
Alopecia Areata Incognita: The Bottom Line
Alopecia areata incognita can be a distressing and confusing condition, especially when it mimics other types of hair loss.
However, with early recognition, a thorough diagnostic approach, and individualized treatment, many patients experience meaningful improvement and even full regrowth.
Emotional support and reliable resources can further help you regain confidence and peace of mind. With the right care, you can take control of your hair health and move forward with hope. You're not alone on this journey—there is a path to recovery from alopecia areata incognita.
Talk to a board-certified dermatologist to discuss your goals and find the solution that is best for you.
Frequently Asked Questions
Is alopecia areata incognito reversible?
Yes, alopecia areata incognita is reversible, especially with early diagnosis and treatment. Many patients respond well to corticosteroids or immunotherapy, and full regrowth is possible, though recurrence may occur depending on underlying triggers.
What is the difference between androgenic alopecia and alopecia areata incognita?
Androgenic alopecia causes gradual thinning in specific patterns and is linked to hormones. Alopecia areata incognita, by contrast, causes rapid, diffuse shedding with minimal visible patches and is autoimmune in nature, often requiring a different treatment approach.
How to disguise alopecia areata?
Options for disguising alopecia areata include using volumizing products, root touch-up powders, wigs, or hair toppers. Some patients also benefit from strategic haircuts and styling techniques. Dermatologists can also recommend cosmetic camouflage or scalp micropigmentation as an option.
What are triggers for alopecia areata?
Triggers for alopecia areata may include physical or emotional stress, infections, hormonal changes, certain medications, or autoimmune flare-ups. Genetics also plays a role, and identifying potential triggers can help guide both treatment and prevention strategies.