A scalp biopsy is a simple yet powerful diagnostic tool that can uncover the hidden causes behind unexplained hair loss or scalp conditions.
Whether you’re dealing with sudden shedding, thinning patches, or persistent irritation, a biopsy can provide clear answers when other tests fall short. For many patients, it’s the first step toward an accurate diagnosis and an effective hair thinning treatment solution.
We’ll walk you through everything you need to know about scalp biopsies for hair loss, including how they work, what they can detect, how to prepare, and what to expect before and after the procedure, so you can approach your appointment with confidence and peace of mind.
What Is a Scalp Biopsy?
A scalp biopsy is a minor, minimally invasive dermatological procedure used to diagnose the underlying cause of hair loss or scalp disorders when the clinical exam alone isn’t conclusive.
During the procedure, a small sample of scalp tissue—usually 4 mm in diameter—is removed and examined under a microscope.
Dermatologists may recommend a scalp biopsy when patients present with unexplained hair thinning, patchy bald spots, scarring, or signs of inflammation.
It’s especially helpful in distinguishing between scarring (cicatricial) and non-scarring alopecias, such as lichen planopilaris, alopecia areata, or telogen effluvium.
A scalp biopsy can also help diagnose infections, autoimmune conditions such as lupus, or other inflammatory skin diseases affecting the scalp.
This diagnostic tool provides critical information that helps rule out conditions with similar symptoms and helps determine the best personalized treatment options.
Types of Scalp Biopsy Procedures
There are three main types of scalp biopsy procedures: punch biopsy, elliptical biopsy, and shave biopsy.
- A punch biopsy uses a circular blade to remove a core of tissue, usually from the area of active hair loss.
- An elliptical biopsy involves removing an oval-shaped strip of scalp, often when a larger sample is needed.
- A shave biopsy removes only the upper layers of skin and is less common for hair loss evaluation, but may be used for surface lesions.
The most popular scalp biopsy methods are punch and excisional biopsies. The choice between these methods depends on the size and location of the area being sampled and the suspected diagnosis.
What Can a Scalp Biopsy Detect?
A scalp biopsy for hair loss is a powerful diagnostic tool that can detect a wide range of hair and scalp conditions, especially when clinical examination and patient history are inconclusive.
By examining both the skin and hair follicles microscopically, dermatopathologists can identify the presence, pattern, and depth of inflammation, scarring, and follicular damage.
Common conditions diagnosed through scalp biopsy include:
- Alopecia areata – an autoimmune disorder where the immune system attacks hair follicles.
- Lichen planopilaris and frontal fibrosing alopecia – scarring types of hair loss linked to inflammation and immune activity.
- Telogen effluvium – diffuse shedding due to stress or systemic triggers.
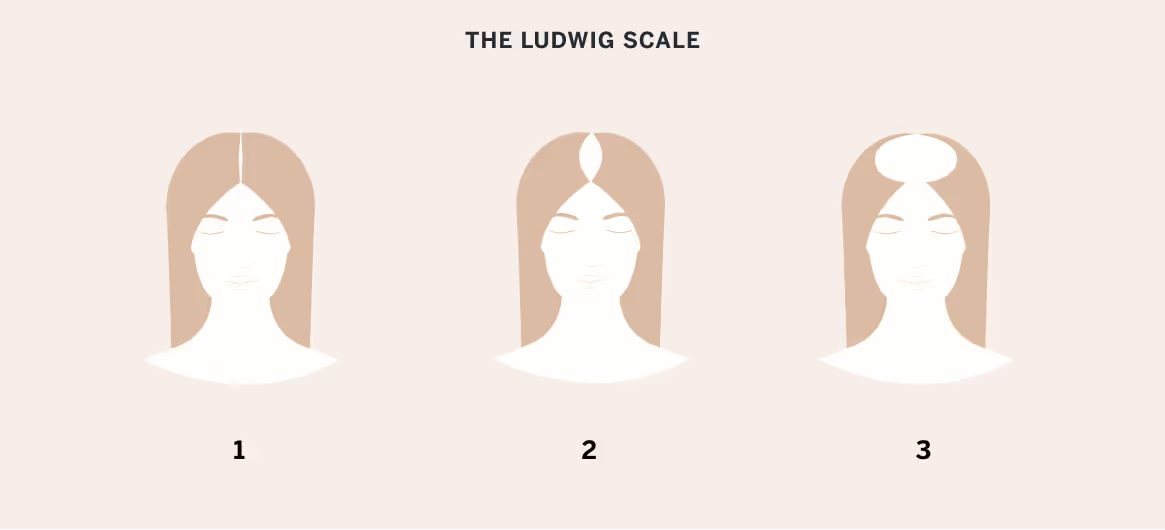
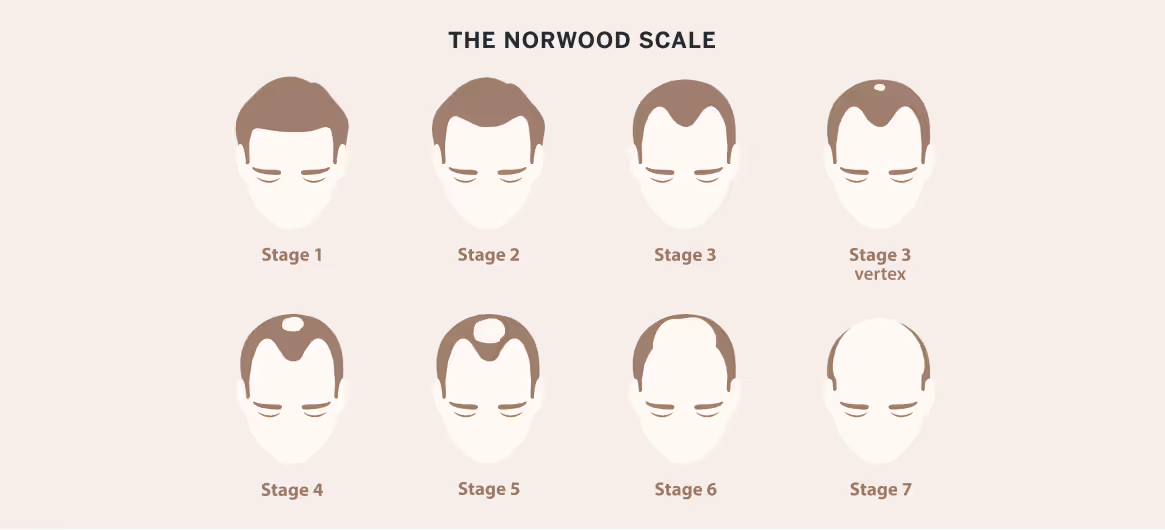
- Androgenic alopecia (pattern hair loss) – follicular miniaturization with increased telogen-to-anagen ratio. It’s usually diagnosed clinically, but a biopsy can confirm the diagnosis by ruling out other issues.
- Discoid lupus erythematosus – an autoimmune condition causing inflammation and scarring.
- Folliculitis decalvans – a neutrophilic inflammatory disorder causing permanent hair loss.
- Fungal or bacterial infections – such as tinea capitis or folliculitis.
A scalp biopsy can also help confirm or rule out skin cancer, psoriasis, and other dermatologic conditions affecting the scalp.
One important distinction a scalp biopsy can make is between scarring and non-scarring types of alopecia. Scarring alopecia, also known as cicatricial alopecia, occurs when hair follicles are destroyed and replaced by scar tissue.
Non-scarring alopecia, such as alopecia areata or telogen effluvium, involves hair loss without permanent follicle damage. Identifying the type of alopecia is essential for determining the appropriate treatment plan.
How To Prepare for a Scalp Biopsy
Proper preparation helps ensure a smooth biopsy experience and accurate diagnostic results. Your dermatologist will give specific instructions based on your health history and the area to be sampled. You may need to adjust medications, pause certain hair products, and plan for aftercare.
Medications and Products To Avoid
You may be advised to stop taking blood thinners, NSAIDs (such as ibuprofen), or supplements that increase bleeding risk.
Avoid applying topical corticosteroids, minoxidil, or harsh hair treatments for at least a few days before the procedure, as these can alter biopsy results or delay healing.
Steps To Take Before Your Appointment
Wash your hair with a gentle shampoo the night before or morning of the biopsy, but do not use conditioner or styling products. Eat normally unless instructed otherwise. Arrange for a ride if you’re prone to lightheadedness or are receiving sedating medications.
What To Expect During a Scalp Biopsy Procedure
During a scalp biopsy for hair loss, the doctor will clean the area to be biopsied and inject a local anesthetic to numb the skin. Using a punch tool or scalpel, they will remove a small sample of skin and hair follicles. The sample will be placed in a sterile container and sent to a laboratory for analysis.
The doctor will apply pressure to the biopsy site to stop any bleeding and may place a few stitches to close the wound. A bandage may be applied in some cases to protect the area as it heals.
Most patients experience minimal discomfort during a scalp biopsy, thanks to the local anesthetic. You may feel a slight pinch or pressure as the sample is taken, but it shouldn't be painful.
After the procedure, you might experience some mild soreness or tenderness at the biopsy site, which can be managed with over-the-counter pain relievers.
Scalp Biopsy Aftercare and Healing
To ensure proper healing, keep the biopsy site clean and dry. Your doctor will provide specific instructions on how to care for the wound, which may include gently cleaning the area and applying an antibiotic ointment.
If bleeding continues after you leave the office, use sterile gauze to apply constant pressure to the area until bleeding ceases. Avoid scratching or picking at the scab that forms over the biopsy site.
If stitches were used to close the biopsy site, your doctor will schedule a follow-up appointment to remove them, usually within 7–14 days. They will also advise you on when it's safe to resume normal activities, such as washing and styling your hair or exercising.
Signs of Infection or Complications
Watch for signs of infection, such as increasing redness, warmth, swelling, pus, or worsening pain at the biopsy site. Fever or swollen lymph nodes may also indicate complications.
Rare issues include delayed healing, allergic reactions to sutures or antiseptics, and scarring, especially in patients prone to keloids. If you experience any of these symptoms or develop a fever, contact your doctor immediately.
Does Hair Grow Back After Scalp Biopsy?
In most cases, hair regrows at the biopsy site within a few months, especially if no scarring occurs.
However, if a scarring alopecia is present or if the sample site heals with a small scar, regrowth may be limited or absent in that exact spot. Surrounding hair typically remains unaffected.
Risks and Side Effects of Scalp Biopsy
As with any invasive procedure, there is a risk of bleeding and scarring. However, these risks are minimal with a scalp biopsy, and most patients experience only minor, temporary discomfort. The biopsy site may leave a small scar, but this is usually hidden by surrounding hair growth.
There is a slight risk of infection following a scalp biopsy, but this can be minimized by properly caring for the biopsy site and following your doctor's aftercare instructions. If an infection does occur, it can typically be treated with antibiotics.
How Accurate Is a Scalp Biopsy for Hair Loss Diagnosis?
A scalp biopsy is considered the gold standard for diagnosing hair loss conditions. It provides detailed information about the health of hair follicles and the scalp's overall condition, allowing doctors to make an accurate diagnosis and develop an effective treatment plan.

Alternatives to Scalp Biopsy for Hair Loss Diagnosis
While a scalp biopsy provides valuable diagnostic information, dermatologists often begin with less invasive methods. These alternatives can help identify the cause of hair loss in many cases, but a biopsy may still be needed to confirm a diagnosis:
- Clinical examination – Visual inspection and pattern recognition often suggest common types of hair loss, such as androgenic alopecia.
- Pull test and tug test – These assess active shedding or hair fragility.
- Trichoscopy (dermoscopy) – A magnified view of the scalp reveals follicular patterns and signs of inflammation or miniaturization.
- Blood tests – Help detect hormonal imbalances, thyroid issues, nutrient deficiencies, and autoimmune markers.
- Hair counts and phototrichograms – Quantify shedding and regrowth.
Moving Forward After a Diagnosis
Once a diagnosis is confirmed, your dermatologist will recommend a personalized treatment plan based on the underlying cause of your hair loss.
The goal is to slow progression, stimulate regrowth when possible, and support long-term scalp health. Both medical and lifestyle interventions may be part of your care.

Prescription Medications
Prescription treatments can be highly effective, particularly for androgenic alopecia and certain inflammatory conditions.
- Topical or oral minoxidil helps extend the growth phase of hair follicles.
- Finasteride products and dutasteride products, which are 5-alpha-reductase inhibitors, reduce dihydrotestosterone (DHT), a key factor in pattern hair loss.
- Spironolactone products, an antiandrogen, is often prescribed for women with hormonally driven hair thinning.
- In scarring alopecias, corticosteroids or immunosuppressants may be used to control inflammation.
Your dermatologist may also recommend platelet-rich plasma (PRP) therapy or low-level laser therapy (LLLT) as complementary options to enhance results, especially when used alongside medical treatments.
Lifestyle Changes To Support Hair Growth
In addition to prescription treatments, several lifestyle changes can support healthier hair growth and scalp function, enhancing medical outcomes and helping preserve hair health long term:
- Balanced nutrition – Ensure adequate intake of iron, protein, vitamin D, and other key vitamins and nutrients.
- Stress management – Practices such as yoga, meditation, or cognitive behavioral therapy may reduce shedding linked to stress.
- Gentle hair care – Avoid harsh brushing, heat styling, and tight hairstyles that cause traction.
- Consistent scalp hygiene – Use mild shampoos, and avoid buildup that can clog follicles.
- Regular follow-ups – Ongoing dermatologic care helps track progress and adjust treatments as needed.
A Scalp Biopsy Can Lead to Solutions!
Facing hair loss can feel overwhelming, but a scalp biopsy is a small step that can lead to major answers. The procedure is quick, safe, and often the key to uncovering the root cause of persistent or unexplained hair thinning.
Many patients find peace of mind simply by having a clear diagnosis and a plan of action. With today’s advanced treatments and the guidance of a skilled dermatologist, there is real hope for stabilizing hair loss and promoting regrowth.
If you’ve been struggling without answers, a scalp biopsy may be the turning point in your journey to healthier hair.
Talk to a board-certified dermatologist to discuss your goals and find the solution that is best for you.
Frequently Asked Questions
How painful is a scalp biopsy?
The pain associated with a scalp biopsy is generally mild. Local anesthesia is used to numb the area before taking the biopsy, which minimizes discomfort during the procedure. Some soreness may occur afterward, but it's usually manageable with over-the-counter pain relief.
Why would a dermatologist do a scalp biopsy?
A dermatologist may perform a scalp biopsy to identify the cause of hair loss or scalp abnormalities. It helps diagnose conditions such as alopecia areata, scarring alopecia, psoriasis, inflammatory conditions, or infections that can’t be determined through a visual exam alone.
Do they shave your head for a scalp biopsy?
Shaving the entire head isn’t necessary for a scalp biopsy. The dermatologist may trim or shave a small section, usually less than a quarter inch, at the biopsy site to properly access the scalp. Hair usually shows signs of regrowth in the area within a few weeks after healing.
Can a scalp biopsy show lupus?
Yes, a scalp biopsy can help detect cutaneous lupus erythematosus or systemic lupus if it’s affecting the skin or hair follicles. The procedure allows dermatopathologists to identify inflammation and immune activity associated with lupus-related hair loss.