Glucocorticoids are steroid-based anti-inflammatory medications that help reduce redness, swelling, and irritation in the scalp—factors that can worsen hair loss. By binding to the glucocorticoid receptor, these medications suppress overactive immune responses and calm inflammation that can damage follicles.
However, not everyone responds to glucocorticoids in the same way. A variant in the NR3C1 gene, known as rs6198, influences how sensitive your glucocorticoid receptors are. Depending on your genetic profile, you may experience normal responsiveness, reduced sensitivity, or even genetic resistance to these treatments.
The Role of Genetics in Glucocorticoid Response
The NR3C1 gene encodes the glucocorticoid receptor, which mediates the effects of steroid medications. The rs6198 variant can change the stability and function of this receptor, impacting how well it binds to and is activated by glucocorticoids.
- High responsiveness means the receptor binds effectively, and steroidal anti-inflammatory treatments are expected to work as intended.
- Moderate sensitivity suggests the receptor is less efficient, so you may see a diminished effect of steroidal treatment.
- Genetic resistance occurs when the receptor’s altered function prevents the drug from working at a clinically meaningful level.
Understanding your NR3C1 genotype allows you and your healthcare provider to make more targeted treatment choices—potentially avoiding wasted time on less effective options.
Tailored Recommendations by Efficacy Level
Based on your genotype, your likelihood of responding to steroidal anti-inflammatory treatments may vary—these strategies are tailored to your specific genetic profile.
Top Strategies for High Steroid Effectiveness
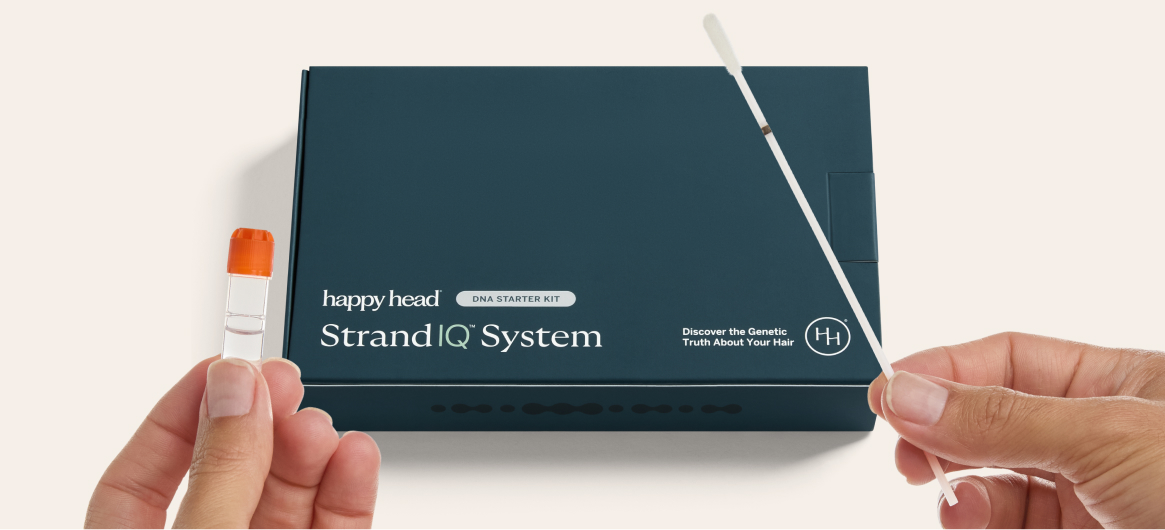
If your Happy Head StrandIQ™ analysis indicates normal glucocorticoid responsiveness, these medications can be effective for managing scalp inflammation.
- Use for targeted inflammation
Your healthcare provider can prescribe topical steroids to address localized redness and swelling. - Integrate long-term support
Non-steroidal anti-inflammatories such as cetirizine or piroxicam gel can help manage ongoing issues without prolonged steroid use. - Combine strategically
In flare-ups, pairing steroids with other anti-inflammatory or antifungal agents may speed recovery.
Approaches for Moderate Steroid Effectiveness
If your genetic profile suggests some reduction in glucocorticoid sensitivity, focus on short-term, targeted use and combination strategies.
- Limit steroid exposure
Use for brief, targeted applications rather than as a long-term solution. - Boost results with combinations
Pair steroids with antifungals, salicylic acid, or antihistamines to improve inflammation control. - Assess progress regularly
Monitor scalp condition and consult with your provider to determine if alternative primary treatments might be needed.
Low Likelihood of Effectiveness or Glucocorticoid Resistance
When your NR3C1 variant predicts significant resistance, glucocorticoids may provide minimal benefit.
- Avoid as primary treatment
Skip steroids as a first-line therapy for scalp inflammation. - Prioritize non-steroidal approaches
Use NSAIDs, COX or COX-2 inhibitors, or immune-modulating topical treatments for more consistent results. - Explore complementary therapies
Incorporate antioxidant-rich scalp care and anti-inflammatory nutrition strategies to support follicle health.
Choosing the Right Path Forward
Your genetic makeup plays a direct role in determining how well steroidal anti-inflammatory medications work for you. By matching your NR3C1 profile to the right treatment approach—whether it’s standard steroid therapy, combination regimens, or steroid alternatives—you can address scalp inflammation more effectively and protect long-term hair health.
Resources
StrandIQ SNP Marker Count: 1
StrandIQ Genes for Trait:
NR3C1
References:
Botelho Barra, C., et al. (2022). Pharmacogenomic markers of glucocorticoid response in congenital adrenal hyperplasia. PLoS One, 17(12), e0279298. PMID: 36538565.
Nordkap, L., et al. (2022). Hair cortisol, glucocorticoid gene receptor polymorphisms, stress, and testicular function. Psychoneuroendocrinology, 146, 105942. PMID: 36179533.
Oakley, R.H., Cidlowski, J.A. (2013). The biology of the glucocorticoid receptor: new signaling mechanisms in health and disease. Journal of Allergy and Clinical Immunology, 132(5), 1033–1044. PMID: 24084075.
Ramirez-Falcon, M., et al. (2024). Defining the differential corticosteroid response basis from multiple omics approaches. International Journal of Molecular Sciences, 25(24), 13611. PMID: 39769372.
Sombetzki, C., et al. (2025). Impact of glucocorticoid receptor polymorphism rs6198 on sepsis survival in a prospective multicenter cohort. Scientific Reports, 15(1), 24760. PMID: 40634451.
Štampar, P., et al. (2024). Genetic variability in the glucocorticoid pathway and treatment outcomes in hospitalized patients with COVID-19: a pilot study. Frontiers in Pharmacology, 15, 1418567. PMID: 39135792.
Strehl, C., et al. (2019). Glucocorticoids—all-rounders tackling the versatile players of the immune system. Frontiers in Immunology, 10, 1744. PMID: 31396235.
This content, including StrandIQ™ DNA analysis reports and any Happy Head products and/or services referenced therein, is for informational and cosmetic purposes only. It is not intended to diagnose, treat, cure, or prevent any disease. This content does not constitute medical advice and should not be used to make healthcare decisions. References to prescription treatments are educational in nature. Always consult a licensed healthcare professional for any medical concerns or treatment decisions.