The Ludwig Scale is a widely used system for classifying female pattern hair loss, helping dermatologists identify the extent and progression of thinning.
Unlike male baldness patterns, women often experience diffuse thinning across the mid-scalp, making an accurate assessment essential for effective treatment.
By understanding where you fall on the scale, both you and your dermatologist can make informed decisions about proven hair growth medications, therapies, lifestyle adjustments, and monitoring, increasing the likelihood of preserving density and achieving meaningful hair regrowth.
What Is the Ludwig Scale of Classification?
The Ludwig Scale is a clinical classification system developed in the 1970s by Dr. Erich Ludwig to accurately describe patterns of female pattern hair loss (FPHL).
Before its introduction, most diagnostic tools were based on male baldness patterns, which did not reflect how women typically experience thinning.
The Ludwig Scale reorganized the approach by focusing on density loss along the part, diffuse thinning across the mid-scalp, and progressive visibility of the underlying scalp.
It outlines three clearly defined stages, allowing dermatologists to quantify severity, document progression, and select treatments more precisely.
Its creation marked a turning point in understanding FPHL as its own condition, improving diagnostic consistency, guiding research, and helping clinicians tailor therapies to a patient’s specific pattern and degree of thinning.
The Three Stages of the Ludwig Scale
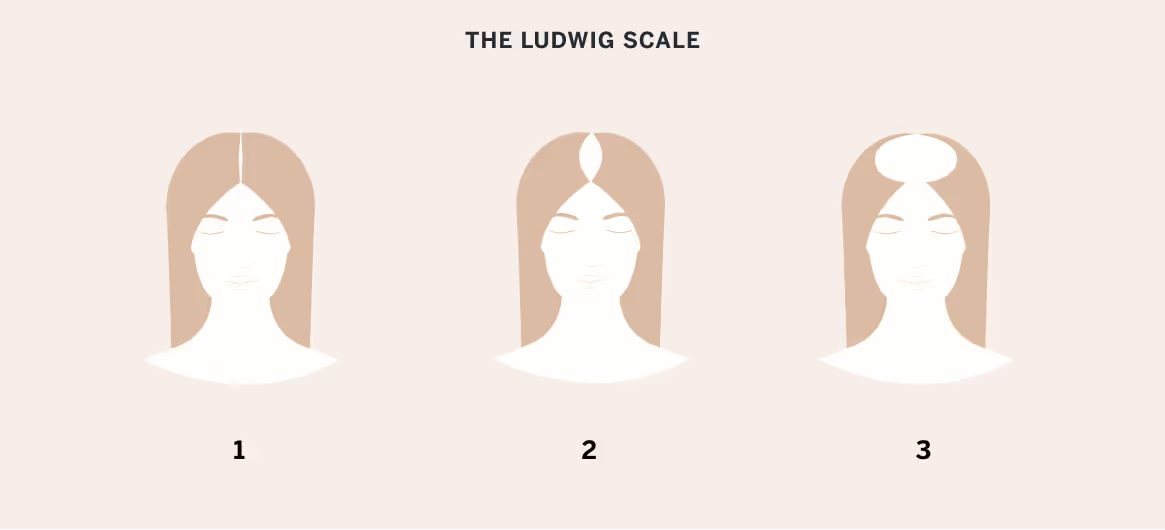
The Ludwig Scale divides female pattern hair loss into three progressive stages, each reflecting increasingly visible thinning through the mid-scalp.
These stages help describe what patients actually see and experience day to day, from subtle changes in density to pronounced loss at the crown.
Stage I: Thinning Along Part
Stage I represents early female pattern hair loss and often begins as a subtle widening of the central part. Density is reduced, but the scalp is not prominently visible, making the change easy to overlook or attribute to aging, stress, or postpartum shifts.
Many women first notice that familiar hairstyles, such as a straight center part or smooth ponytail, suddenly look “flatter” or expose more scalp under bright light.
Clinically, follicles are miniaturizing, yet many remain functional, making this the most responsive stage to treatment.
Treatment at Stage I focuses on preservation and strengthening existing hair. Dermatologists often recommend topical minoxidil, prescription-strength formulations, nutritional evaluation, and gentle styling habits to reduce breakage.
Happy Head's Custom Topical Rx Solution, containing minoxidil with retinoic acid, works particularly well for early intervention, and the StrandIQ DNA Starter Kit helps personalize treatment by identifying which ingredients will work best based on individual genetics.
Early intervention during Stage I can help preserve density, improve coverage, and slow the rate of miniaturization before the loss progresses into more noticeable thinning.
Stage II: Scalp Visibility
Stage II involves more noticeable thinning across the mid-scalp, with the part widening enough that the scalp becomes visible in various lighting conditions.
Patients frequently report difficulty achieving volume, increased time spent camouflaging the area, and frustration that hair fibers or volumizing products no longer offer the same coverage.
Dermatologically, the number of miniaturized follicles increases, and overall density decreases, making the pattern easier to identify during clinical examination.
Stage II responds well to combination therapies. Happy Head’s topical spironolactone for women, which combines spironolactone, minoxidil, retinoic acid, and hydrocortisone in a specialized solution formula, addresses multiple pathways of hair loss simultaneously.
Adding the SuperCapsule with oral finasteride, minoxidil, and vitamin D3 creates a comprehensive approach. The Laser Helmet Growth System can provide additional stimulation to dormant follicles, making it an excellent adjunct therapy for this stage.
At this stage, addressing coexisting factors, such as thyroid imbalance, iron deficiency, and hormonal fluctuations, is particularly important. Consistent treatment can still improve density and slow visible progression.
Stage III: Crown Baldness
Stage III is the most advanced form of female pattern hair loss on the Ludwig Scale and is characterized by pronounced thinning or near-complete loss at the crown with significant scalp visibility.
Hair surrounding the affected region may also appear limp or sparse, creating styling limitations that make concealment difficult even with strategic parting, toppers, or cosmetic fibers.
Although follicles are highly miniaturized, many remain alive, meaning they may still respond to combination therapy.
Dermatologists typically use a multi-modal approach, combining prescription topical treatments, oral medications, PRP, and device-based therapies to preserve remaining follicles.
Some patients may also explore procedural options such as hair transplantation if they have a suitable donor supply. Emotional impact is common at this stage, making supportive guidance and long-term management essential.
Ludwig Scale vs. Sinclair Scale
The Ludwig Scale and the Sinclair Scale both classify female pattern hair loss, but they differ in structure, sensitivity, and clinical use.
The Ludwig Scale uses three broad stages focused on mid-scalp thinning and crown visibility, making it ideal for documenting moderate to advanced loss.
The Sinclair Scale offers five gradations, allowing dermatologists to detect milder, earlier changes that might not fit neatly into Ludwig categories. Many clinicians use both systems together to monitor subtle progression and tailor treatment intensity more precisely.

What Causes Hair Loss in Women?
Hair loss in women can result from a combination of genetic, hormonal, environmental, and medical factors.
The most common cause is female pattern hair loss, which is driven by follicular sensitivity to androgens and progressive miniaturization.
Hormonal shifts, such as those occurring during menopause, postpartum periods, thyroid disorders, or polycystic ovary syndrome, can accelerate shedding or unmask underlying genetic thinning.
Nutrient deficiencies (iron, zinc, or vitamin D), chronic inflammation, and autoimmune conditions such as alopecia areata can also contribute.
Certain medications, crash dieting, major illness, and high stress may trigger telogen effluvium, causing diffuse shedding. Additionally, chemical processing, heat damage, and tight hairstyles can exacerbate thinning.
Because many of these factors overlap, a thorough dermatologic evaluation is essential for accurate diagnosis and targeted treatment.
Assessing Your Stage at Home
Self-assessment using the Ludwig Scale requires good lighting, a handheld mirror, and ideally someone to help photograph hard-to-see areas.
Start by parting your hair down the middle as you normally would, and then examine the width of the part line from your forehead to the crown.
Creating a consistent documentation system helps you track changes over time. Take photos monthly from multiple angles: directly above, from each side, and from behind.
Use the same lighting conditions and camera distance each time. Mark your calendar for these photo sessions to maintain consistency. Compare images side by side every three months to identify subtle changes that daily observation might miss.
Home evaluation, however, has limits. Lighting, styling, and hair texture can distort what you see.
If you notice persistent widening of the part, visible scalp in multiple lighting conditions, or rapid shedding, a professional dermatologic assessment is recommended to confirm the diagnosis and rule out treatable medical causes.
The Importance of Early Detection
Early detection is critical because female pattern hair loss progresses through a gradual miniaturization process in which genetically susceptible follicles shrink over successive growth cycles.
As follicles miniaturize, they produce finer, shorter hairs with reduced pigmentation until they eventually become barely visible vellus strands.
Intervening early helps interrupt this process while many follicles are still active and capable of producing thicker terminal hairs. Prompt treatment can preserve density, improve coverage, and slow long-term progression before scalp visibility becomes pronounced.
Identifying changes, such as a widening part or decreased volume, early allows dermatologists to tailor therapies that stabilize follicles and maximize regrowth potential.
Treatments for Female Pattern Hair Loss
Treating female pattern hair loss requires a multi-layered approach that addresses both follicular miniaturization and the underlying hormonal or genetic drivers.
Dermatologists typically combine medications, procedures, and supportive strategies to protect active follicles and encourage thicker, more resilient regrowth.

Topical Solutions and Oral Medications
- Minoxidil: Minoxidil products increase blood flow to follicles, prolong the growth phase, and can thicken miniaturized hairs over time. Prescription-strength topical solutions or low-dose oral minoxidil are often first-line treatments. Consistency is essential, as results typically appear after three to six months and continue to improve with ongoing use.
- Finasteride: Though more commonly used in men, prescription finasteride products can be prescribed for select postmenopausal women. It reduces dihydrotestosterone (DHT), the hormone that drives follicle miniaturization. Dermatologists carefully evaluate candidacy due to hormonal considerations.
- Dutasteride: A stronger 5-alpha-reductase inhibitor, prescription dutasteride blocks more DHT-producing pathways than finasteride. It may be considered in advanced cases or when other therapies are insufficient.
- Spironolactone: Widely used in women, prescription spironolactone products help counteract androgen-related thinning by blocking androgen receptors. It can reduce shedding and improve density, particularly in women with signs of hormonal imbalance or early-onset pattern thinning. Regular monitoring of potassium and blood pressure is recommended.
Microneedling, LLLT, and PRP Therapy
Microneedling creates controlled micro-injuries that stimulate growth factors and enhance absorption of topical treatments such as minoxidil.
Low-level laser therapy (LLLT) improves cellular energy production within follicles, supporting thicker regrowth when used consistently.
PRP therapy involves injecting concentrated platelet-derived growth factors to strengthen miniaturized follicles and reduce shedding. These therapies are often combined with medications to boost density, especially in mild to moderate female pattern hair loss.
Lifestyle Changes
Addressing lifestyle factors helps optimize treatment outcomes by reducing triggers that accelerate thinning.
- Ensuring adequate iron, vitamin D, and protein supports hair cycling, while stress-management techniques can reduce telogen shedding.
- Gentle styling, avoiding tight hairstyles, minimizing heat exposure, and spacing out chemical treatments preserve fragile strands.
- Maintaining overall hormonal and metabolic health through balanced nutrition, sleep, and routine medical care creates a more favorable environment for regrowth and long-term stability.
Hair Transplants
Hair transplantation may be an option for select women with stable female pattern hair loss and sufficient donor density at the occipital scalp.
Modern follicular unit extraction (FUE) and follicular unit transplantation (FUT) techniques allow surgeons to redistribute permanent follicles to thinning mid-scalp or crown areas.
Results and recovery depend on realistic expectations, adequate donor supply, and careful evaluation to rule out diffuse unpatterned alopecia. Transplants are most successful when combined with ongoing medical therapy to protect remaining native hair.
Using the Ludwig Scale To Guide Treatment
The Ludwig Scale does more than describe hair loss; it gives women a practical framework for recognizing meaningful changes early and seeking timely care.
When paired with a thorough dermatologic evaluation, it can reveal underlying contributors, guide personalized treatment, and help track progress with clarity.
Most importantly, it reminds patients that female pattern hair loss is manageable and that meaningful improvement is possible when evidence-based therapies are used consistently and monitored over time.
Talk to a board-certified dermatologist to discuss your goals and find the solution that is best for you.
Frequently Asked Questions
What is the Ludwig Scale of hair loss?
The Ludwig Scale is a medical classification system used to describe female pattern hair loss. It categorizes thinning into three distinct stages, focusing on how density decreases along the part, the extent of visible scalp, and eventual crown thinning to guide diagnosis and treatment.
How is the Ludwig Scale used in hair loss treatment?
Dermatologists use the Ludwig Scale to determine the severity of thinning, monitor progression, and select appropriate therapies. By identifying a patient’s stage, clinicians can tailor treatment intensity, track response over time, and adjust therapies such as medications, procedures, or adjunctive care.
Can hair grow back from female pattern baldness?
Hair can often regrow or become noticeably thicker with proper treatment, especially when addressed early. While female pattern baldness is chronic and progressive, options such as minoxidil, oral medications, and in-office therapies can stabilize loss, improve density, and support long-term maintenance.
Is there anything that really works for female hair loss?
Yes. Evidence-based treatments include topical and oral medications, microneedling, low-level laser therapy, and PRP therapy. These options can slow shedding, stimulate regrowth, and improve coverage when used consistently. Success depends on early intervention, correct diagnosis, and a personalized plan.