Did you know that two-thirds of men will experience some degree of hair loss by age 35?
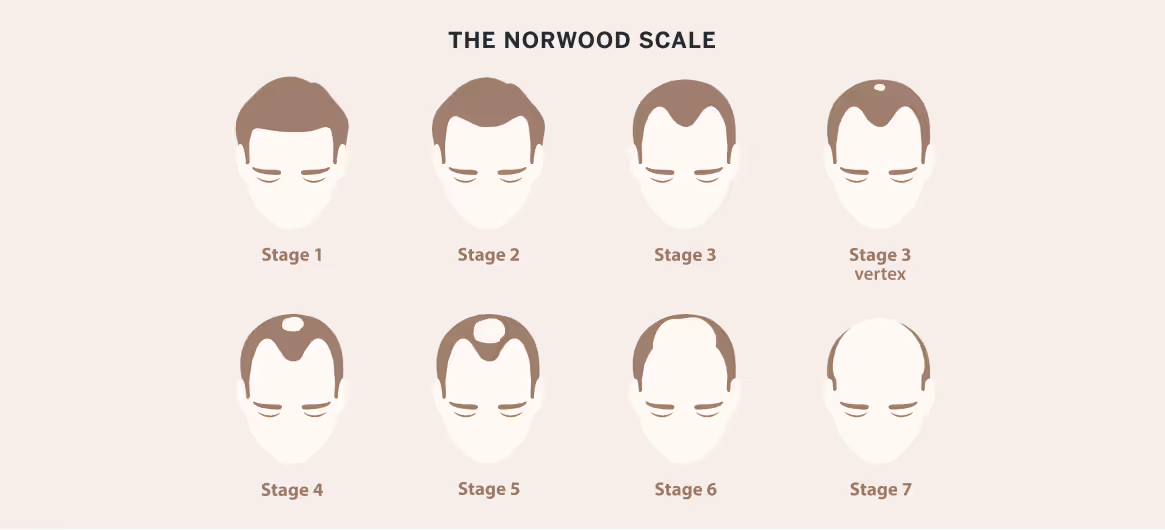
The Norwood scale serves as the standard classification system that doctors use to measure male pattern baldness progression. This seven-stage framework helps identify where you stand regarding your hair loss.
Once you know your stage, you can track changes over time and make informed decisions about treatment before hair loss becomes more advanced.
Working with a dermatologist gives you access to personalized guidance and proven hair loss solutions that can help slow thinning, maintain your hair, and support regrowth.
What Is the Norwood Scale?
The Norwood Scale is a standardized classification system used to describe the progression of male pattern baldness, also known as androgenetic alopecia.
First developed in the 1950s and refined by Dr. O’Tar Norwood in the 1970s, the Norwood Scale organizes hair loss into seven distinct stages based on predictable patterns of recession and thinning.
Dermatologists use the scale to document severity, track changes over time, guide treatment decisions, and set realistic expectations for outcomes.
Its consistency makes it a valuable clinical and research tool, allowing providers to communicate clearly about the extent and trajectory of hair loss.
Seven Stages of Hair Loss
The Norwood Scale outlines hair loss as a predictable, stepped progression, making it easier to understand how androgenetic alopecia changes over time.
Each stage reflects specific patterns of recession and thinning that help dermatologists determine severity and guide appropriate treatment planning.
Stage 1
Stage 1 represents a full, intact hairline with no measurable recession at the temples. Density across the frontal, mid-scalp, and crown remains normal, and there are no clear indicators of male pattern baldness.
Men may notice natural maturing of the hairline, but this is not considered active androgenetic alopecia.
Stage 2
Stage 2 involves mild, symmetric recession at the temples, forming an early M-shaped contour. Density is still strong across the rest of the scalp, and crown thinning is generally absent.
While not classified as balding, this stage may signal the earliest visible changes associated with hereditary hair loss in genetically susceptible individuals.
Stage 3
Stage 3 marks the first stage officially defined as balding. Temple recession deepens, creating a more pronounced M- or V-shaped hairline.
Some individuals also develop Stage 3 Vertex (also called 3A), characterized by a distinct thinning or small bald spot at the crown. This stage indicates more significant follicle miniaturization driven by DHT sensitivity.
Stage 4
Stage 4 shows further temple recession and a more visible, enlarged bald spot at the crown. A band of hair typically still separates the front and crown, but it becomes noticeably thinner.
Follicle miniaturization is more advanced, and untreated individuals often begin to experience faster, more predictable progression toward mid-scale hair loss patterns.
Stage 5
Stage 5 features substantial frontal recession and an expanding crown area that begins narrowing the band of hair between them. Although still present, this bridge is thinner and weaker than in Stage 4.
The shape of the balding areas becomes more rounded due to more extensive androgen-driven follicular decline.
Stage 6
Stage 6 represents the merging of the frontal and crown bald areas, leaving no significant hair bridge between them.
The remaining hair on the top of the scalp becomes sparse, with thinning extending into the mid-scalp. Only the sides and back retain density, forming the classic horseshoe pattern typical of advanced androgenetic alopecia.
Stage 7
Stage 7 is the most advanced stage on the Norwood Scale, characterized by severe loss across the entire top of the scalp. Only a narrow band of hair remains around the sides and back, and even this zone may show some degree of thinning.
Treatment options become more limited, and restoration typically focuses on maximizing remaining donor resources for a possible hair transplant.
Assessing Hair Loss at Home
Assessing hair loss at home requires good lighting, a handheld mirror, and a second mirror or smartphone camera to view hard-to-see areas. Natural light or bright overhead lighting helps show subtle thinning.
Gently parting the hair in multiple areas can help you compare density and identify early miniaturization patterns. Photograph your hairline, temples, mid-scalp, and crown every few months to help you spot gradual changes.
Front Hairline Changes
When examining the front hairline, look for symmetrical temple recession, increasing curvature of the M- or V-shape, and reduced density along the frontal band.
Compare older photos to identify subtle shifts, such as widening gaps between hairs or a more transparent appearance under bright light. Pay attention to whether the hairline is maturing naturally or showing patterned recession consistent with early androgenetic alopecia.
Crown Thinning Patterns
To evaluate the crown, use two mirrors or a smartphone held above the head to assess the swirl area where thinning typically begins. Look for widening of the natural cowlick, increased scalp visibility, or a circular zone of reduced density.
Because crown loss can progress slowly and unevenly, reviewing photos taken months apart will help you spot early miniaturization or the formation of a distinct thinning patch.
How Dermatologists Use the Norwood Scale To Diagnose Hair Loss
Dermatologists use the Norwood Scale as part of a structured diagnostic process to determine the severity and pattern of androgenetic alopecia.
The appointment typically begins with a thorough medical, family, and medication history to identify genetic risk and rule out contributing conditions.
During the exam, the dermatologist evaluates the hairline, temples, mid-scalp, and crown, comparing these patterns to standardized Norwood stages. Dermoscopy may be used to assess miniaturization, follicular density, and inflammation.
Providers also look for signs of alternative diagnoses such as telogen effluvium, alopecia areata, or scarring alopecias. In some cases, bloodwork or a scalp biopsy may be needed to clarify the cause. The Norwood Scale then guides treatment planning and long-term monitoring.

What Causes Male Pattern Baldness?
Male pattern baldness, or androgenetic alopecia, is caused by a combination of genetics, hormones, and age-related changes in follicle sensitivity.
The primary driver is dihydrotestosterone (DHT), a hormone that binds to susceptible follicles and gradually shortens their growth cycle. Over time, affected follicles produce finer, shorter hairs—a process called miniaturization—until they eventually stop producing visible hair.
Genetics determines how sensitive each follicle is to DHT and which areas of the scalp are affected. Age further accelerates this process as follicular regeneration slows.
While male pattern baldness is not a sign of poor health, underlying factors such as nutritional deficiencies, stress, or certain medications can worsen visible thinning.
Can Male Pattern Baldness Be Prevented?
Male pattern baldness cannot be fully prevented because follicular sensitivity to DHT is genetically determined. However, early intervention can significantly delay progression.
Evidence-based therapies, such as finasteride, minoxidil, and low-level laser devices, help preserve density and slow miniaturization.
Maintaining overall health, reducing stress, and addressing nutritional deficiencies may further support hair quality, though they cannot override hereditary androgen sensitivity.
When To See a Dermatologist for Hair Loss
A dermatologist should be consulted when you notice persistent shedding, a receding hairline, crown thinning, or a clear change compared with older photos. Early evaluation is important because treatments work best before significant miniaturization occurs.
Additional warning signs, such as patchy loss, scalp irritation, rapid shedding, or a family history of early baldness, warrant prompt professional assessment to confirm the cause and begin targeted therapy.
Treatment Options for Norwood Scale Stages 1–7
Managing male pattern baldness requires a tailored approach based on where a patient falls on the Norwood Scale.
Because follicle miniaturization progresses over time, early, consistent, evidence-based treatment offers the best chance to preserve density and support visible regrowth.

Early Stages (Norwood Scale 1–3)
In the early stages, the goal is to slow miniaturization and preserve existing density. Topical or oral minoxidil products can stimulate growth, while finasteride and/or dutasteride reduce DHT to protect vulnerable follicles. Patients with mild recession often respond well to combination therapy.
Low-level laser devices and supportive treatments, such as microneedling, may further enhance outcomes. Early intervention typically yields the most noticeable improvement.
Mid Stages (Norwood Scale 4–5)
At this level, both the frontal hairline and crown show more established thinning. Prescription oral finasteride or dutasteride is often recommended because systemic DHT reduction provides stronger protection for widespread miniaturization.
Minoxidil helps maximize growth potential in remaining follicles. Some patients may benefit from PRP therapy or microneedling to boost response. Hair transplantation may be considered if medical therapy alone cannot achieve the desired coverage.
Late Stages (Norwood Scale 6–7)
In advanced stages, the top of the scalp has extensive loss, making medical therapy primarily a maintenance strategy. Oral dutasteride or finasteride may help retain remaining hair along the transition zones, while minoxidil supports any viable follicles.
Hair transplantation becomes the primary restorative option, though donor availability must be carefully assessed. Adjunctive therapies such as PRP can improve graft survival and enhance overall cosmetic results when used alongside surgery.
Using the Norwood Scale To Guide Your Next Steps
Understanding the Norwood Scale empowers you to take a proactive approach to hair loss. By identifying your stage, you can make informed decisions about treatment options, set realistic expectations, and track progress over time.
Don’t wait to seek help. Early recognition and intervention maximize results, and regular monitoring helps adjust strategies as hair loss evolves.
Consulting a dermatologist ensures personalized guidance, whether pursuing medical therapy, procedural options, or lifestyle measures to preserve and restore hair.
Talk to a board-certified dermatologist to discuss your goals and find the solution that is best for you.
Frequently Asked Questions
Is Norwood Scale 2 balding?
Norwood 2 shows mild, patterned recession at the temples that forms an early M-shaped hairline. While it isn’t classified as true balding, it may represent the earliest visible stage of androgenetic hair loss. Tracking changes and seeking a dermatologist’s evaluation can help determine whether treatment is appropriate.
Is Norwood 3 too late?
Norwood 3 is the first stage formally recognized as balding. It is marked by deeper temple recession and visible thinning. Although progression is more apparent, it is not too late for meaningful improvement. Evidence-based treatments such as minoxidil, finasteride, or combination therapies can slow loss and often stimulate measurable regrowth.
How do I know my Norwood scale?
You can estimate your stage by comparing your temples, frontal hairline shape, and crown density with the standardized Norwood diagrams. Look for consistent patterns such as symmetrical recession or a widening bald spot. Because self-assessment can be imprecise, a dermatologist can confirm your stage and identify the underlying cause.
Is losing 700 hairs a day normal?
Shedding roughly 700 hairs daily is well above the average 50–100 shed hairs per day and usually signals an active hair loss process, such as telogen effluvium or progressing androgenetic alopecia. If shedding at this level continues for several weeks, a dermatologist should evaluate potential triggers, perform testing, and recommend appropriate treatment.